In late January 2012, Caitlin Cahow, two-time Olympic women's and professional hockey player, Harvard graduate and law student, suffered a concussion while fighting for the puck along the boards during a women's professional hockey game.
Diagnosed with a concussion, she returned a month later, but was injured again, the crushing blindside hit causing a concussion so serious that, as she later posted on her Facebook page, she was left her unable "to read, remember, think clearly, go outside without dark glasses, or stand for 5 minutes without debilitating headaches, dizziness, and crippling fatigue."
Cahow remembered being unable to get out of bed for two weeks, losing 25 pounds from not eating, and suffering persistent headaches. Despite the fact that she didn't like taking any medications, not even Advil, her medicine cabinet was filled with pain meds.
It was then that I got a call from one of Caitlin's teammates to ask me to "do anything I could to help her get medical care." Who did I think would help her the most, I was asked.

It was a tricky question to answer, but I knew from years of watching the USA Women's Ice Hockey team, and getting to know many of its players (among them, fellow Harvard players, Angela Ruggiero and Julie Chu) (that's me with Caitlin at Fenway Park at the 2010 Winter Classic), how many hits such tough young ladies take to the helmet, and how much they get banged around (in a sport which technically doesn't allow body checking!). That her teammate had come to me meant that the career of one of the players I enjoyed so much watching during my trip to the Olympic Winter Games in Vancouver was in serious jeopardy. Talking with Caitlin and hearing about the tough shape she was in gave me a bad headache, too!
When conventional therapies for post-concussion syndrome didn't seem to helping, Caitlin, as she later told USA Today,[1] had what amounted to an epiphany: she remembered thinking about her mom and the most cherished people in her life, walked outside, threw all the meds in a dumpster, and resolved to try to take a different approach to her symptoms of post-concussion syndrome.
Moving from Boston to her parent's house on an island off the coast of Maine, she took a year off from law school, worked on a lobster boat, and, finally, went to see Ted Carrick, a chiropractic neurologist and founder of the Carrick Institute in Atlanta, Georgia. Caitlin's visit to the Carrick Institute was facilitated by her agent, Brant "Senator" Feldman, to whom Caitlin and her family will be forever grateful for his support on her road to recovery. [If Carrick's name sounds familiar, he is best known for helping Pittsburgh Penguin star, Sidney Crosby, return to the ice after PCS]
By October 2012, Cahow was back playing for the Boston Blades, captaining the team, which won the Clarkson Cup in the Canadian Women's Hockey League, but, after being left off the roster for the U.S. team that won the world's championships in April 2013, she decided to retire rather than accept an invitation to try out for her third Olympic team. 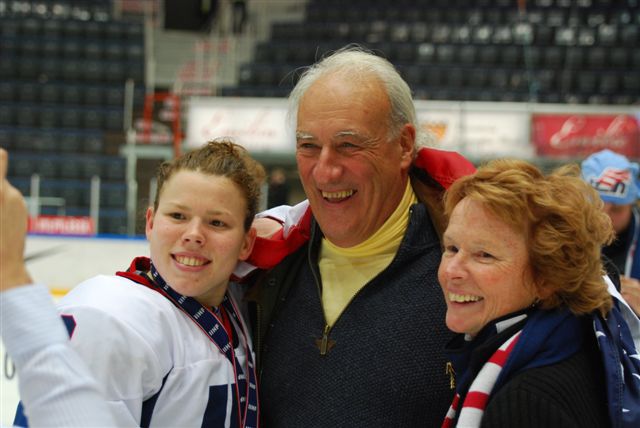
A mom's perspective
Through all of her dark days, Caitlin's mother, Barbara Kinder, herself a surgeon, was there for her. Here are what Barbara told me about Caitlin's treatment and her recovery from her unique perspective as both mother and physician:
"1. Every concussion is unique. Every concussion is different from every other. 'One size fits all' evaluation and treatment will not work. For the same reason, it is not easy to prove treatment efficacy by means of controlled, randomized studies, the 'gold standard' for evaluating new therapies. Promising new treatments can be (and are) sometimes unfairly dismissed as not meeting these standards when the complexity/variability of post concussion syndromes makes it hard to construct comparable groups to look at aggregate outcomes of possible different treatments.
2. Computerized neurocognitive testing doesn't help in treatment. The development of computerized neurocognitive tests such as ImPACT have been a big advance in terms of making sure an athlete has recovered their cognitive function necessary to return to play or work, but the usual and primary treatment remains rest, with follow-up testing using the ImPACT paradigm, and return to play or work following the algorithm of the ImPACT program based on test results.
3. Multi-disciplinary teams are hard to assemble. Those suffering from PCS experience a wide variety of symptoms, commonly including fatigue, depression, anxiety, sensitivity to bright lights and noise, inability to read, look at a computer or TV, and a sense of isolation and hopelessness. (as Caitlin lamented, "I miss my mind and my body.") Experts thus emphasize the importance of employing a team of specialists. In my experience, assembling such a team, however, can be hard to achieve in today's world. Sustained access to providers, even the simple ability to call with a question or concern and get a call back, is critical to optimal recovery. Fortunately, in this respect, the Carrick Institute program was exemplary.
4. Privacy laws can get in the way. HIPAA regulations restrict the ability of parents of children over 18 to have direct access to providers at a time when, as was the case with Caitlin, their child may not be fully able to take charge of his/her own care. That leads parents unable to fully support their child, which adds to the profound sense of isolation patients with post-concussion syndrome experience.
5. A thorough diagnostic evaluation is critical. At the Carrick Institute, Caitlin underwent a comprehensive history and physical exam and a detailed neurological assessment. Among the specialized neurologic evaluations were videonystagmography (VNG), which is designed to test inner ear and central motor functions, and computerized dynamic postural studies (CAPS), which assess the interaction of vestibular, somatosensory and visual systems for patients undergoing neurorehabilitation
6. Individualized therapy essential. Because each concussion is unique, the therapies employed to treat their symptoms of PCS need to be individualized for each patient's situation based fter initial evaluation. Such therapies can include vision exercises, left brain exercises, on-ice-tailored drills, cold laser therapy, gyrostim treatments, and cranial nerve stimulation. Again, some of these treatments are being used by mainstream medical specialists such as neurologists (cranial nerve stimulation for migraine) and otolaryngologists (balance issues with gyrostim), but, as of yet, infrequently for post-concussion syndrome. Another important aspect of treatment was the intensive contact with staff, sharing experiences with other patients and their families, and observing the progress of the other patients over the course of a week or two.
I observed remarkable improvement in Caitlin and the other patients in the first week in terms of symptoms, personality, physical and intellectual functioning and objective data like VNG. Consolidation of gains were achieved in those staying for a second week. In subsequent visits as needed "fine-tuning" of residual issues could be achieved by new visual exercises.
7. Follow-up is critical. As with any treatment, especially for conditions that evolve over time, such as rehabilitation from an injury or illness, follow-up is vital for an optimally successful outcome. All patients of the Carrick Institute have what amounts to immediate access to staff and Carrick at all times. Patients' questions are promptly answered, eliminating sources of anxiety and the sense of isolation. Evolving treatment programs are designed as indicated."
Barbara's final thoughts
"Medicine is both a pragmatic (evolving practice by "what works") and an intellectual (building knowledge by hypothesis driven investigation) pursuit. It is inherently conservative - appropriately so - in order to ensure that new treatments are safe and effective. There are many examples of theoretically sound treatments which , after greater use, were found to be not only ineffective, but dangerous."
"On the other hand, sometimes conservatism can hinder the development and more widespread use of important treatments. This is especially a problem in today's highly specialized world of medicine, where communication between specialties about promising treatment modalities may be limited. It is always easier to do what we have always been doing pretty successfully than to keep checking "outside the box" for something that might work better."
"In my field of surgery, it took decades for the technology of laparoscopic surgery to move from gynecology, where it was first introduced, to general surgery, and then to use in general surgery, and then to surgery in general. You could say that this was the biggest development since anesthesia, but it had to overcome professionally entrenched opposition to become the standard of care it is today."
"I suspect that some of this conservatism will need to be overcome to bring these promising techniques of diagnosis and treatment into the mainstream of concussion management."
"Fortunately, for my daughter Caitlin, and for other parents with kids who suffer from symptoms of post-concussion syndrome, I think it is already happening."
Need comprehensive concussion information? Visit our Concussion Center.
1. Kelly Whiteside. One year later, Caitlin Cahow's life back to normal following concussion scare. USA Today (August 26, 2013)(http://www.usatoday.com/story/sports/olympics/2013/08/26/concussion-hock...)(accessed October 13, 2013).
Posted October 16, 2013